PCOS can make weight loss a challenging journey, but with the right approach and determination....
Read more1. Introduction to PCOS and ACNE
Polycystic Ovary Syndrome (PCOS) is a complex and prevalent hormonal disorder that affects individuals of reproductive age. While PCOS is renowned for its primary association with fertility issues, it often presents a multifaceted array of symptoms and challenges. Among these challenges, one of the most frequently encountered is ACNE.
ACNE, a skin condition marked by the presence of pimples, blackheads, and other blemishes, can affect individuals of all ages and genders. However, those with PCOS are particularly susceptible to developing ACNE due to the intricate interplay of hormones within their bodies.
1.1 Understanding Hormonal Imbalances
- Hormonal Imbalance: At the heart of the connection between PCOS and ACNE lies hormonal imbalances. PCOS disrupts the typical hormonal harmony within the body, leading to a surge in the production of androgens, commonly referred to as "male hormones." These androgens are present in both males and females but tend to be elevated in individuals with PCOS. An excess of androgens can instigate various skin-related issues, with ACNE being one of the most visible manifestations.
- Role of Hormones: To delve deeper into this connection, it's essential to recognize the crucial role that hormones play in regulating skin health. Hormones, including estrogen, progesterone, and testosterone, significantly influence the skin's physiology. Imbalances in these hormones can lead to changes in sebum production, skin cell turnover, and inflammation—all of which contribute to the development of ACNE lesions.
1.2 The Role of Inflammation
- Influence of Androgens: Beyond the direct influence of androgens on sebum production, these hormones also impact keratinocytes, the cells responsible for skin cell turnover. In individuals with PCOS, androgens can stimulate keratinocytes to produce excess keratin, a protein that can combine with sebum to form plugs within hair follicles. These plugs, known as comedones, are the hallmark of non-inflammatory ACNE lesions.
- Insulin Resistance: In addition to hormonal factors, insulin resistance is another crucial player in the development of ACNE in individuals with PCOS. Insulin is a hormone responsible for regulating blood sugar levels. In PCOS, insulin resistance occurs, causing the body to produce higher levels of insulin to maintain stable blood sugar. Unfortunately, elevated insulin levels can trigger the ovaries to produce more androgens, further exacerbating hormonal imbalances. This insulin-driven increase in androgens contributes to the development and persistence of ACNE.
1.3 The Impact of Sebum Production
- Sebum and ACNE: Sebum, an oily substance produced by sebaceous glands, plays a pivotal role in the development of ACNE. Androgens, particularly dihydrotestosterone (DHT), stimulate these sebaceous glands to produce more sebum. While sebum is essential for maintaining skin hydration, excessive sebum production can lead to several skin issues, including ACNE.
- Formation of Comedones: In individuals with PCOS, the overproduction of sebum can create an environment where hair follicles become clogged more easily. The combination of excess sebum and keratin within hair follicles can lead to the formation of comedones, the precursors of ACNE lesions. Comedones can manifest as whiteheads or blackheads on the skin's surface.
- Role of Bacteria: Moreover, the accumulation of excess sebum within hair follicles provides an ideal environment for the proliferation of Propionibacterium ACNEs (P. ACNEs), a type of bacteria that naturally resides on the skin. When P. ACNEs multiply within clogged hair follicles, they trigger an inflammatory response from the body's immune system. This inflammation, coupled with the presence of sebum, leads to the formation of inflammatory ACNE lesions, such as papules, pustules, nodules, and cysts.
1.4 The Role of Genetics
- Genetic Predisposition: While hormones and insulin resistance are central to the development of ACNE in PCOS, genetics also play a role. Some individuals may have a genetic predisposition to developing ACNE-prone skin. This genetic influence can impact various aspects of skin physiology, including sebum production, keratinocyte activity, and inflammatory responses.
- Genetic Susceptibility: In individuals with PCOS who have a genetic susceptibility to ACNE, the combination of hormonal imbalances and insulin resistance can exacerbate their skin condition. Therefore, understanding the genetic factors contributing to ACNE in PCOS can aid in personalized treatment and management strategies.
1.5 Psychological and Emotional Impact
- Emotional Struggles: Beyond the physical challenges posed by ACNE in PCOS, it's essential to acknowledge the psychological and emotional impact it can have. ACNE can significantly affect an individual's self-esteem, body image, and overall quality of life. The visible nature of ACNE lesions can lead to feelings of self-consciousness and embarrassment.
- Mood Disturbances: These emotional struggles are often compounded by the hormonal fluctuations and mood disturbances commonly associated with PCOS. The emotional toll of ACNE can lead to increased stress, anxiety, and depression, further exacerbating the condition.
Understanding the holistic impact of ACNE in PCOS is crucial for comprehensive care. Effective management strategies encompass not only the physical aspects of ACNE but also the emotional and psychological well-being of individuals living with PCOS.
2. Causes and Triggers of PCOS-Related ACNE
2.1 Hormonal Imbalances
Hormonal imbalances, particularly elevated levels of androgens, are a hallmark of PCOS and a primary driver of ACNE in affected individuals. The complex interplay of hormones within the body sets the stage for ACNE development.
- Androgen Dominance: In PCOS, there is an overproduction of androgens, including testosterone and dihydrotestosterone (DHT). Elevated androgen levels can lead to increased sebum production, a key contributor to ACNE development.
- Impact on Follicles: Androgens also affect hair follicles, making them more prone to becoming clogged with sebum and keratin. This process leads to the formation of comedones, the initial stages of ACNE lesions.
- Menstrual Cycle Influence: The hormonal fluctuations throughout the menstrual cycle can exacerbate ACNE in individuals with PCOS. Specific phases of the cycle can lead to heightened androgen levels, intensifying sebum production and ACNE breakouts.
2.2 Insulin Resistance
Insulin resistance, a common feature of PCOS, is closely linked to ACNE development. Elevated insulin levels in the bloodstream play a significant role in worsening ACNE symptoms.
- Hyperinsulinemia: Insulin resistance leads to hyperinsulinemia, a condition characterized by high levels of insulin. This excess insulin stimulates the ovaries to produce more androgens, contributing to hormonal imbalances and ACNE.
- Proinflammatory Effects: Insulin resistance is associated with chronic low-grade inflammation, which can exacerbate ACNE. Inflammation promotes the formation of inflammatory ACNE lesions and worsens existing ones.
- Effect on Skin Cells: Insulin resistance can also affect the skin's keratinocytes and sebaceous glands, further promoting ACNE development. It leads to increased keratin production and sebum secretion, both of which are ACNE triggers.
2.3 Genetics
Genetics play a significant role in determining an individual's susceptibility to ACNE. While not everyone with PCOS experiences ACNE, certain genetic factors can increase the likelihood of developing ACNE-prone skin.
- Familial Tendencies: If ACNE-prone skin runs in your family, you may be more likely to experience ACNE, especially in the presence of PCOS-related hormonal imbalances.
- Genetic Variations: Certain genetic variations can impact sebum production, skin cell turnover, and inflammation—key factors in ACNE development. Understanding your genetic predisposition can help tailor ACNE management strategies.
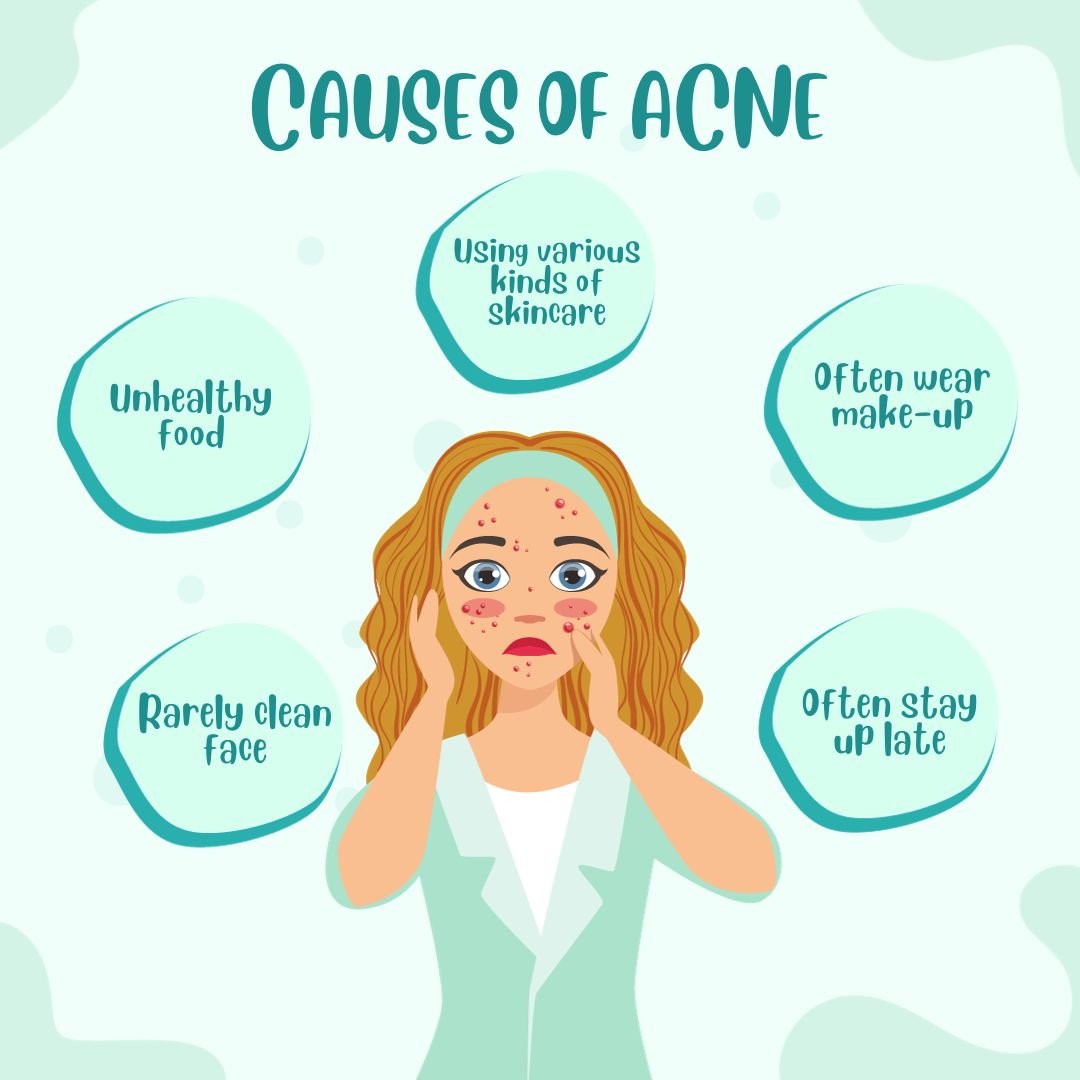
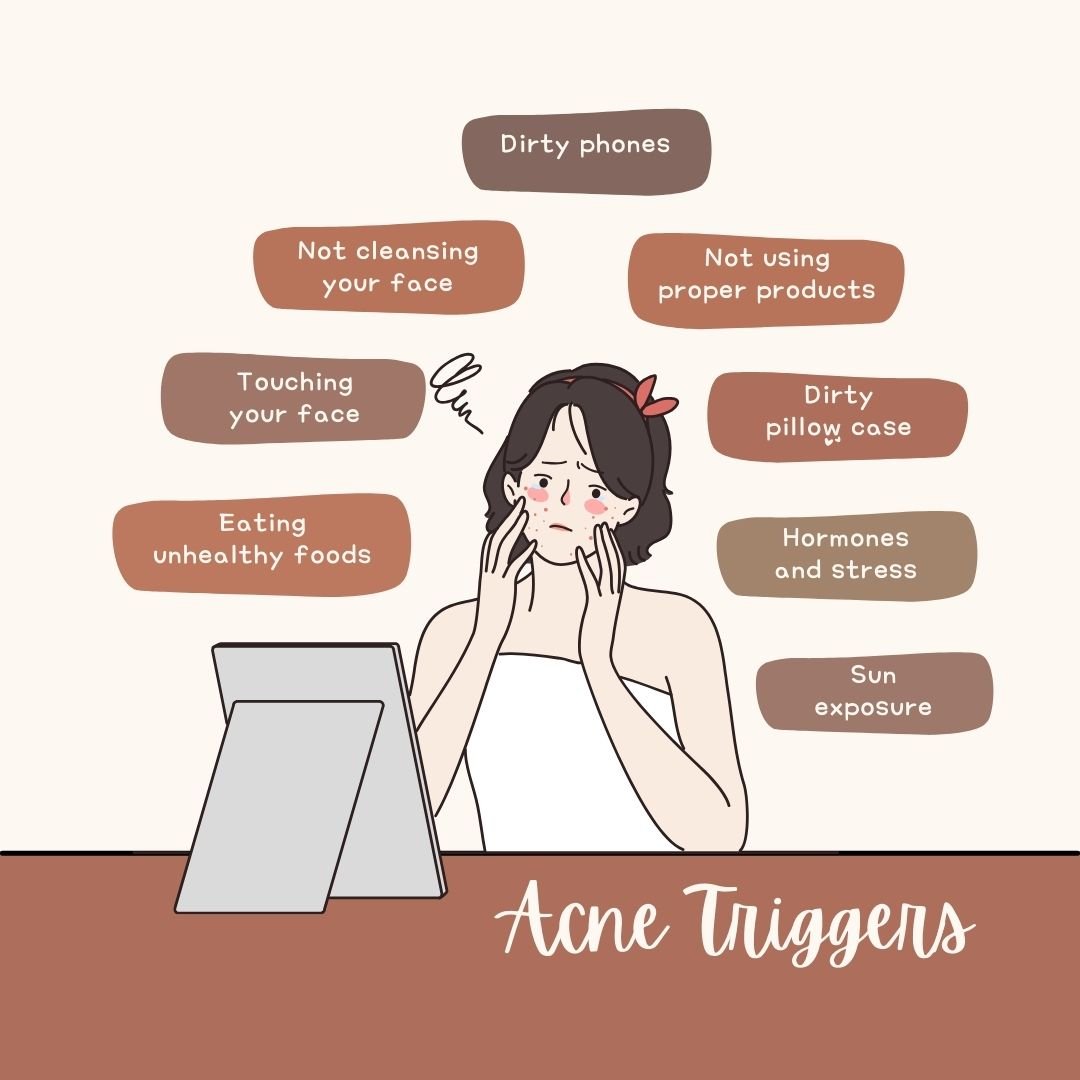
2.4 Lifestyle Factors
Lifestyle factors can significantly influence the severity of ACNE in individuals with PCOS. Making informed choices in various aspects of daily life can help manage and reduce ACNE symptoms.
- Dietary Choices: Poor dietary habits can exacerbate ACNE. Consuming high-glycemic foods and dairy products, for example, can increase insulin levels and worsen hormonal imbalances, contributing to ACNE breakouts.
- Stress: Chronic stress can trigger hormonal changes and inflammation, both of which can worsen ACNE. Stress management techniques are essential for individuals with PCOS-related ACNE.
- Skincare Habits: The choice of skincare products and routines can impact ACNE. Using non-comedogenic (non-pore-clogging) products and adopting a suitable skincare regimen is crucial.
In summary, ACNE in individuals with PCOS is the result of a complex interplay between hormonal imbalances, insulin resistance, genetics, and lifestyle factors. Recognizing these causes and triggers is the first step toward effective ACNE management.
3. Symptoms and Manifestations of PCOS-Related ACNE
ACNE in individuals with PCOS can present with a range of symptoms and manifestations, often varying in severity and type. Understanding these symptoms is crucial for both diagnosis and effective management.
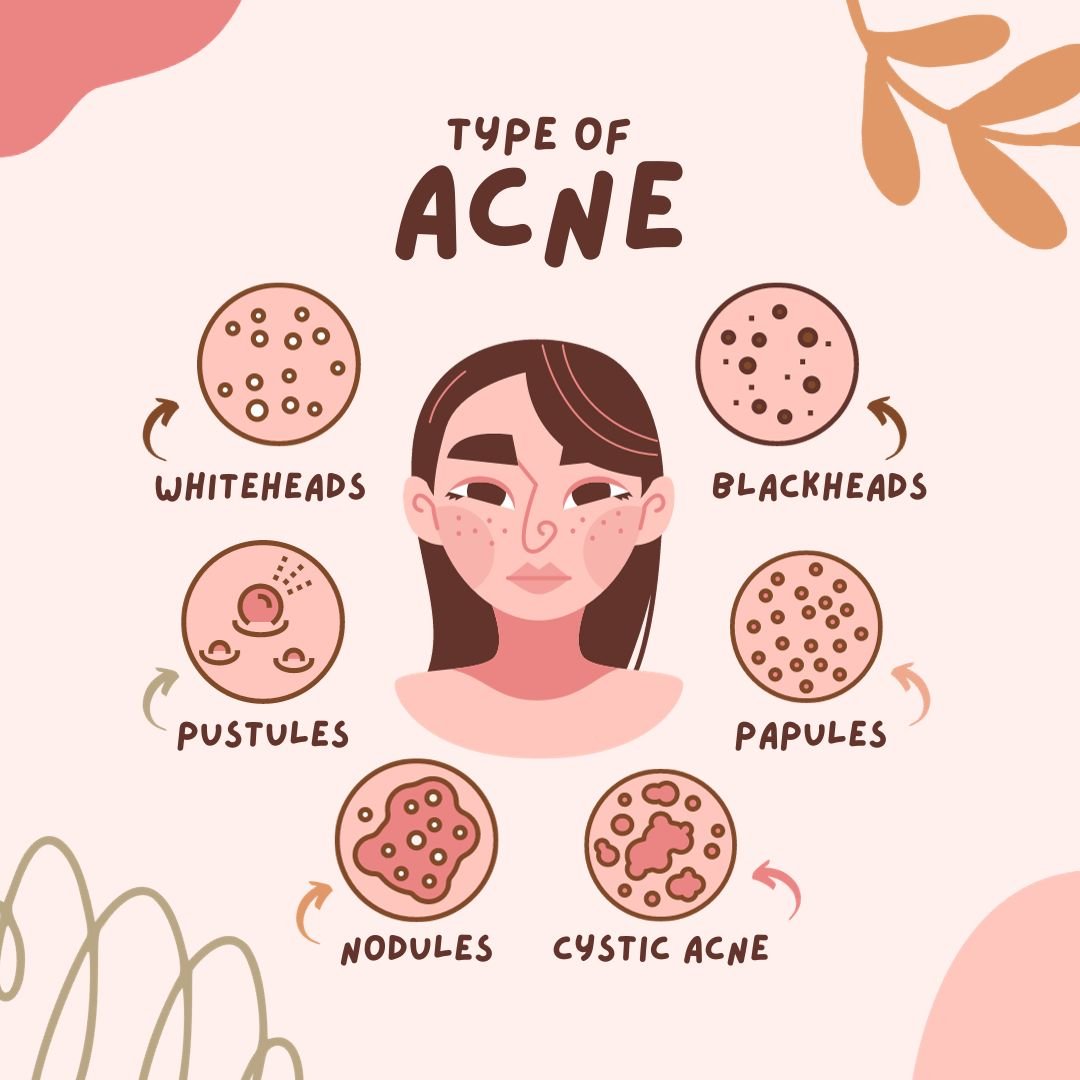
3.1 Types of ACNE Lesions
PCOS-related ACNE typically manifests in the following types of lesions:
- Comedones: These are non-inflammatory ACNE lesions and can be further categorized into open comedones (blackheads) and closed comedones (whiteheads).
- Papules: Papules are small, raised, and often pink or red in color. They result from inflammation and may be tender to the touch.
- Pustules: Pustules are similar to papules but contain pus. They appear as white or yellowish bumps with a red base.
- Nodules: Nodules are larger, solid, and painful lumps beneath the skin's surface. They can be deep-seated and require professional treatment.
- Cysts: Cysts are severe, inflammatory ACNE lesions filled with pus. They are the most painful and can lead to scarring.
3.2 Distribution of ACNE
The location of ACNE breakouts can provide insights into the underlying causes and hormonal influences:
- Facial ACNE: ACNE on the face is common, including the forehead, cheeks, and chin. It may be more prevalent in individuals with PCOS due to increased sebum production in these areas.
- Back and Chest ACNE: Some individuals with PCOS may experience ACNE on their back and chest, which can be especially bothersome.
- Jawline and Neck ACNE: Hormonal fluctuations in PCOS can contribute to ACNE along the jawline and neck.
- Scalp ACNE: ACNE can extend to the scalp, leading to discomfort and sometimes hair loss.
3.3 Associated Symptoms
In addition to visible ACNE lesions, individuals with PCOS-related ACNE may experience other associated symptoms:
- Pain and Discomfort: Inflammatory ACNE lesions, such as papules, pustules, nodules, and cysts, can be painful and uncomfortable.
- Psychological Impact: ACNE can have a significant psychological and emotional impact, leading to reduced self-esteem, anxiety, and depression.
- Scarring: Severe ACNE lesions, if left untreated, can lead to scarring, which may be permanent.
- Hyperpigmentation: Post-inflammatory hyperpigmentation (dark spots) can persist after ACNE lesions have healed.
- Secondary Infections: Scratching or picking at ACNE can lead to secondary bacterial infections.
Recognizing the various symptoms and manifestations of PCOS-related ACNE is essential for a comprehensive approach to diagnosis and treatment. Addressing both the visible and underlying factors is key to effective ACNE management.
4. Diagnosis and Evaluation of PCOS-Related ACNE
Diagnosing PCOS-related ACNE involves a comprehensive evaluation that considers both the dermatological aspects of ACNE and the underlying hormonal and metabolic factors associated with polycystic ovary syndrome. A healthcare provider may use several methods to diagnose and assess ACNE in individuals with PCOS.
4.1 Clinical Assessment
During a clinical assessment, a healthcare provider will examine the ACNE lesions and assess their type, severity, and distribution. They may also inquire about any associated symptoms, such as pain or discomfort. This visual inspection helps determine the extent of ACNE and its impact on the patient's quality of life.
4.2 Hormonal Evaluation
Hormonal imbalances are a key contributor to PCOS-related ACNE. Therefore, hormonal evaluation is an essential part of the diagnostic process. Tests may include:
- Hormone Blood Tests: Measuring levels of hormones such as testosterone, DHEA-S, LH (luteinizing hormone), and FSH (follicle-stimulating hormone) can provide insights into hormonal imbalances.
- Insulin Levels: Given the connection between insulin resistance and PCOS, measuring fasting insulin levels may be necessary.
- Thyroid Function Tests: Thyroid disorders can sometimes coexist with PCOS and contribute to ACNE. Thyroid function tests may be recommended.
- Anti-Mullerian Hormone (AMH) Levels: Elevated AMH levels are often seen in PCOS and can help in the diagnosis.
4.3 Dermatological Evaluation
A dermatologist may perform a detailed skin examination to assess ACNE severity, identify specific ACNE types (e.g., comedonal, inflammatory, or cystic ACNE), and evaluate any scarring or hyperpigmentation resulting from previous ACNE breakouts.
4.4 Ultrasound Imaging
In some cases, a transvaginal ultrasound may be recommended to evaluate the ovaries. This imaging technique can help identify polycystic ovaries, which are a characteristic feature of PCOS.
4.5 Differential Diagnosis
It's essential to differentiate PCOS-related ACNE from other skin conditions that may present with similar symptoms. These may include hormonal disorders other than PCOS, such as congenital adrenal hyperplasia (CAH) or Cushing's syndrome, and non-hormonal dermatological conditions.
4.6 Psychological Assessment
ACNE can have a significant psychological impact, leading to feelings of self-consciousness and reduced self-esteem. A healthcare provider may conduct a psychological assessment to understand the emotional toll of ACNE and provide appropriate support and counseling.
In conclusion, diagnosing PCOS-related ACNE requires a comprehensive approach that considers clinical, hormonal, dermatological, and psychological aspects. Accurate diagnosis is the first step towards developing a tailored treatment plan to address both the ACNE and the underlying PCOS.
5. Treatment Options for PCOS-Related ACNE

Effectively managing ACNE in individuals with PCOS involves a multi-faceted approach that addresses both the dermatological aspects of ACNE and the underlying hormonal imbalances associated with polycystic ovary syndrome. Treatment options may vary based on the severity of ACNE and individual needs.
5.1 Topical Treatments
Topical treatments are often the first line of defense against PCOS-related ACNE. These include:
- Retinoids: Prescription retinoids, such as tretinoin, can help unclog pores, reduce inflammation, and improve skin texture.
- Topical Antibiotics: Antibacterial creams or gels may be prescribed to target ACNE-causing bacteria and reduce inflammation.
- Azelaic Acid: Azelaic acid is a topical treatment that can help reduce inflammation and improve skin tone.
- Salicylic Acid: This beta hydroxy acid (BHA) exfoliates the skin and can be found in various over-the-counter products.
5.2 Oral Medications
For moderate to severe ACNE, oral medications may be recommended:
- Birth Control Pills: Oral contraceptives can regulate hormonal fluctuations and reduce androgen levels, leading to clearer skin.
- Anti-Androgen Medications: Medications like spironolactone can block the effects of androgens on the skin, reducing ACNE.
- Oral Antibiotics: In some cases, antibiotics may be prescribed to address ACNE-related inflammation.
- Isotretinoin: For severe, treatment-resistant ACNE, isotretinoin may be considered, although it comes with potential side effects and strict monitoring requirements.
5.3 Lifestyle Modifications
Adopting a healthy lifestyle can complement medical treatments and improve ACNE management in PCOS:
- Dietary Changes: A balanced diet with a focus on whole foods and reduced sugar intake can help manage insulin levels and reduce ACNE.
- Regular Exercise: Physical activity can improve insulin sensitivity and promote overall well-being.
- Stress Reduction: Stress management techniques, such as meditation and yoga, can help mitigate stress-related hormonal fluctuations that trigger ACNE.
- Skincare Routine: A consistent skincare routine using non-comedogenic products can help maintain clear skin.
5.4 Dermatological Procedures
In cases of severe ACNE or scarring, dermatological procedures may be considered:
- Chemical Peels: Chemical peels can exfoliate the skin and improve its texture.
- Laser Therapy: Laser treatments can target ACNE and stimulate collagen production to reduce scarring.
- Extraction: Dermatologists can perform ACNE extractions to remove stubborn comedones or cysts.
The choice of treatment for PCOS-related ACNE should be tailored to the individual's needs and preferences. Consulting with a healthcare provider or dermatologist is essential to create a personalized ACNE management plan.
6. Tips for Preventing and Managing PCOS-Related ACNE
Preventing and managing PCOS-related ACNE involves a holistic approach that encompasses skincare, lifestyle modifications, and awareness of hormonal fluctuations. These tips can help individuals with PCOS maintain clearer skin and boost their self-confidence.
6.1 Skincare Routine
A consistent skincare routine can help prevent and manage ACNE:
- Gentle Cleansing: Use a mild, non-comedogenic cleanser to remove dirt, oil, and makeup without stripping the skin.
- Regular Exfoliation: Exfoliate 1-2 times a week to unclog pores and remove dead skin cells.
- Non-Comedogenic Products: Choose skincare and makeup products labeled as non-comedogenic to avoid pore blockage.
- Moisturize: Use a lightweight, oil-free moisturizer to keep the skin hydrated without causing breakouts.
- Sun Protection: Apply sunscreen daily to protect the skin from UV damage and prevent post-inflammatory hyperpigmentation.
6.2 Diet and Nutrition
Your diet can influence ACNE and hormonal balance:
- Low Glycemic Index (GI) Foods: Focus on foods with a low GI to help manage insulin levels. These include whole grains, lean proteins, and vegetables.
- Hydration: Drink plenty of water to keep the skin hydrated and support overall health.
- Omega-3 Fatty Acids: Incorporate sources of omega-3 fatty acids, such as fatty fish and flaxseeds, to reduce inflammation.
- Avoid Sugary and Processed Foods: Limit consumption of sugary and processed foods, which can exacerbate ACNE.
6.3 Regular Physical Activity
Exercise can help manage PCOS and promote clear skin:
- Aerobic Exercise: Engage in regular aerobic activities like brisk walking, cycling, or swimming to improve insulin sensitivity.
- Strength Training: Incorporate strength training exercises to build muscle and support metabolism.
6.4 Stress Management
Stress can exacerbate hormonal imbalances and ACNE:
- Mindfulness Meditation: Practice mindfulness techniques to reduce stress and improve emotional well-being.
- Yoga: Yoga can help manage stress and promote relaxation.
- Breathing Exercises: Incorporate deep breathing exercises into your daily routine to alleviate stress.
Incorporating these tips into your daily life can help you prevent and manage PCOS-related ACNE effectively. However, it's essential to consult with healthcare professionals for personalized guidance and treatment options tailored to your specific needs.
7. Natural Remedies for PCOS-Related ACNE
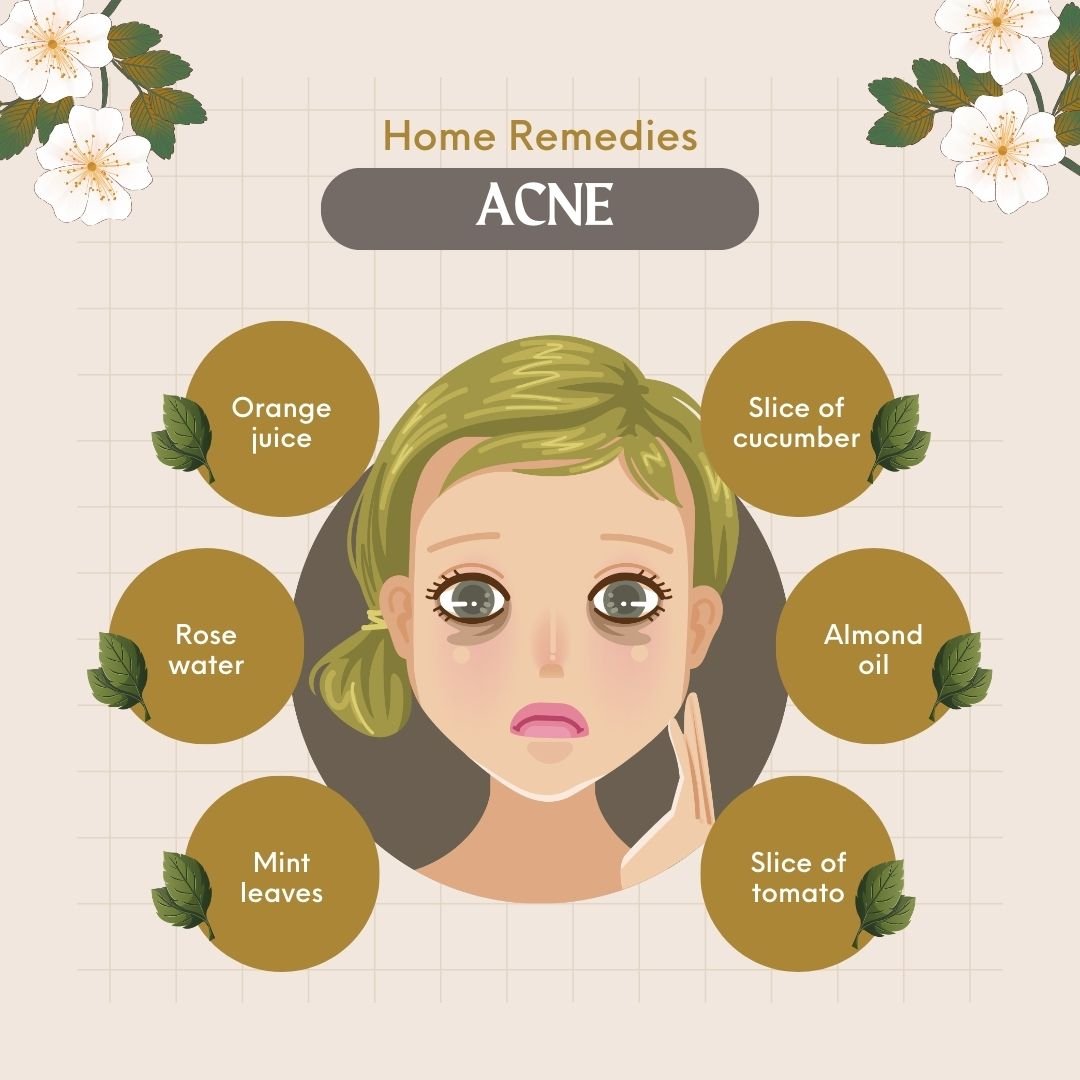
In addition to medical treatments, some individuals with PCOS explore natural remedies to help manage ACNE and promote healthier skin. While these remedies may not be a substitute for medical advice, they can complement your skincare routine and lifestyle modifications.
7.1 Tea Tree Oil
Tea tree oil has natural antibacterial properties and can help reduce ACNE lesions:
- Application: Dilute tea tree oil with a carrier oil (such as jojoba or coconut oil) and apply it directly to ACNE-affected areas.
- Caution: Conduct a patch test before using it on your face to ensure you don't have an adverse reaction.
7.2 Green Tea
Green tea contains antioxidants and anti-inflammatory properties that may benefit the skin:
- Topical Application: Brew green tea, allow it to cool, and use it as a topical toner by applying it to the skin with a cotton ball.
- Oral Consumption: Drinking green tea regularly can provide antioxidants that support overall skin health.
7.3 Aloe Vera
Aloe vera has soothing and anti-inflammatory properties that can help with ACNE-prone skin:
- Gel Application: Apply pure aloe vera gel to ACNE-affected areas to reduce redness and inflammation.
- Hydration: Aloe vera can also help keep the skin hydrated and reduce excess oil production.
7.4 Apple Cider Vinegar
Apple cider vinegar has antimicrobial properties and can help balance the skin's pH:
- Dilution: Mix apple cider vinegar with water (1:3 ratio) and use it as a toner, applying it to the skin with a cotton ball.
- Caution: Ensure proper dilution to avoid skin irritation.
7.5 Honey and Cinnamon Mask
Honey and cinnamon have antibacterial properties and can be used to create a natural face mask:
- Mix: Mix honey and cinnamon powder to create a paste. Apply it to your face, leave it on for 10-15 minutes, and rinse with warm water.
- Hydration: Honey can help retain moisture, while cinnamon has antimicrobial properties.
While these natural remedies have potential benefits for ACNE-prone skin in PCOS, it's crucial to remember that results can vary, and not all remedies may work for everyone. Consulting with a dermatologist or healthcare provider is advisable before trying new treatments, especially if you have sensitive skin or allergies.
8. Lifestyle Changes to Improve PCOS and Skin Health
Making positive lifestyle changes can significantly impact PCOS management and promote healthier skin. These changes address various aspects of life, from diet to stress management, to enhance overall well-being and skin health.
8.1 Balanced Diet
A well-balanced diet can help manage PCOS symptoms and support clear skin:
- Whole Foods: Focus on whole grains, lean proteins, fruits, vegetables, and healthy fats in your diet.
- Portion Control: Be mindful of portion sizes to maintain a healthy weight and improve insulin sensitivity.
- Regular Meals: Eat regular meals and snacks to stabilize blood sugar levels.
8.2 Physical Activity
Incorporating regular physical activity into your routine offers numerous benefits:
- Aerobic Exercise: Engage in aerobic activities like jogging, cycling, or dancing for at least 150 minutes per week.
- Strength Training: Include strength training exercises to build muscle and boost metabolism.
- Consistency: Maintain a consistent workout schedule to see long-term benefits.
8.3 Stress Management
Reducing stress levels can help regulate hormones and improve skin health:
- Meditation: Practice mindfulness meditation to alleviate stress and promote emotional well-being.
- Yoga: Incorporate yoga into your routine for relaxation and stress reduction.
- Breathing Exercises: Engage in deep breathing exercises to manage stress and anxiety.
8.4 Sleep Hygiene
Quality sleep is essential for hormonal balance and skin rejuvenation:
- Consistent Schedule: Aim for a consistent sleep schedule by going to bed and waking up at the same times each day.
- Dark, Quiet Environment: Create a sleep-conducive environment by keeping your bedroom dark and quiet.
- Limit Screen Time: Avoid electronic devices before bedtime to improve sleep quality.
These lifestyle changes, when implemented together, can enhance PCOS management, regulate hormones, and contribute to healthier skin. It's important to consult with healthcare professionals for personalized guidance on making these changes and addressing specific skin concerns.
9. Skincare Tips for PCOS-Related ACNE
Effective skincare practices are essential for managing ACNE associated with PCOS. A tailored skincare routine can help control breakouts, reduce inflammation, and improve skin health. Here are some tips to consider:
9.1 Gentle Cleansing
Start with a gentle cleansing routine to remove dirt, excess oil, and makeup:
- Mild Cleanser: Use a mild, non-comedogenic cleanser twice daily to avoid over-drying the skin.
- Hands Off: Avoid scrubbing or picking at ACNE-prone areas to prevent irritation and scarring.
9.2 Exfoliation
Regular exfoliation can help unclog pores and promote smoother skin:
- Chemical Exfoliants: Consider using chemical exfoliants with ingredients like salicylic acid or glycolic acid to remove dead skin cells.
- Exfoliation Schedule: Limit exfoliation to 1-3 times per week to prevent over-exfoliation.
9.3 Moisturization
Even if you have ACNE-prone skin, proper moisturization is crucial:
- Oil-Free Moisturizer: Opt for an oil-free, non-comedogenic moisturizer to keep your skin hydrated without clogging pores.
- Hydration Balance: Balancing moisture levels can help reduce excessive oil production.
9.4 Sun Protection
Protecting your skin from the sun's harmful UV rays is vital:
- Broad-Spectrum SPF: Use a broad-spectrum sunscreen with an SPF of at least 30 daily, even on cloudy days.
- Avoid Tanning: Tanning can worsen ACNE and lead to skin damage, so avoid excessive sun exposure.
9.5 Makeup Choices
Selecting the right makeup products can prevent pore blockages:
- Non-Comedogenic: Choose makeup labeled as non-comedogenic, meaning it won't clog pores.
- Regular Cleaning: Clean your makeup brushes and sponges regularly to avoid bacteria buildup.
Customizing your skincare routine and following these tips can help manage PCOS-related ACNE and maintain healthier skin. Remember that results may take time, so consistency is key.
10. Consulting a Dermatologist for PCOS-Related ACNE
While self-care and skincare routines can help manage PCOS-related ACNE, it's essential to seek professional guidance when needed. Dermatologists are experts in diagnosing and treating skin conditions, including ACNE associated with hormonal imbalances in PCOS.
10.1 Recognizing When to Consult
Knowing when to consult a dermatologist is crucial for timely treatment:
- Severe ACNE: If you have severe, painful, or persistent ACNE that doesn't respond to over-the-counter treatments, it's time to consult a dermatologist.
- Scarring Risk: If you're at risk of scarring due to ACNE lesions, seeking professional help can prevent long-term skin damage.
- Psychological Impact: ACNE can impact your self-esteem and mental health. If it's affecting your well-being, consult a dermatologist for effective solutions.
10.2 Treatment Options
Dermatologists offer a range of treatment options tailored to your skin type and severity of ACNE:
- Topical Medications: Dermatologists may prescribe topical treatments like retinoids, antibiotics, or benzoyl peroxide to target ACNE.
- Oral Medications: In some cases, oral medications such as antibiotics, hormonal birth control, or isotretinoin may be recommended.
- In-office Procedures: Dermatologists can perform procedures like chemical peels, microdermabrasion, or laser therapy to address ACNE and scars.
10.3 Collaborative Approach
Your dermatologist may work closely with your healthcare provider to address both the hormonal aspects of PCOS and the skincare aspects of ACNE. This collaborative approach ensures comprehensive care.
In conclusion, consulting a dermatologist when dealing with PCOS-related ACNE is a proactive step to achieve clearer, healthier skin. Dermatologists can customize treatment plans based on your unique needs and help you regain confidence in your skin.
Conclusion: Finding the Best PCOS Treatment in Delhi
In the journey to manage PCOS, it's essential to explore various aspects of treatment and support. From understanding the complexities of PCOS to adopting a holistic approach to care, individuals with PCOS can find effective solutions for their unique needs.
While we've discussed numerous strategies and options for managing PCOS, it's important to remember that each person's experience is unique. The best approach to PCOS management often involves a combination of treatments, lifestyle changes, and personalized care.
If you're looking for the best PCOS treatment in Delhi, it's advisable to consult with healthcare professionals who specialize in PCOS management. Delhi offers a range of medical facilities and expert healthcare providers with experience in diagnosing and treating PCOS. To find the best PCOS treatment in Delhi, consider:
- Consulting a Gynecologist: Gynecologists in Delhi are well-equipped to diagnose and provide guidance on PCOS management, including hormonal treatments and fertility options.
- Seeking an Endocrinologist: Endocrinologists specialize in hormonal imbalances and can help address the root causes of PCOS.
- Exploring Fertility Clinics: Fertility clinics in Delhi offer advanced treatments like in vitro fertilization (IVF) and ovulation induction for individuals trying to conceive.
Remember that the best PCOS treatment in Delhi should be tailored to your specific needs and goals. It's essential to have open communication with your healthcare provider and work together to create a personalized treatment plan.
In conclusion, PCOS is a complex condition that requires a multi-faceted approach to care. With the right guidance, support, and access to the best PCOS treatment in Delhi, individuals with PCOS can effectively manage their condition and lead fulfilling lives.